For decades, MRI scans have delivered stunningly beautiful images of the body’s anatomy.
It is now possible to use MRI imaging at cellular level to observe cell metabolism. This is particularly useful in cancer treatment.
With the help of a new technology, doctors may be able to determine on the same day chemo or radiotherapy treatment has been administered whether the treatment works on the cancer cells. This kind of speed is unheard of, as cancer patients normally have to wait months to know whether their treatment is effective.
This new technology is called Hyperpolarized Metabolic MR and was invented by Professor Jan Henrik Ardenkjær-Larsen 15 years ago when he worked at the pharmaceutical company, Nycomed. The Professor is currently heading HYPERMAG, which is located at DTU Electrical Engineering.
“At HYPERMAG, we’re working both to improve the method of hyperpolarization and parts of the MRI technology—including the antennas which receive the signal as well as the collection and processing of data—so that we can produce the best possible images,” says Professor Ardenkjær-Larsen, who originally trained as an electrical engineer.
MRI signal amplified 20,000 times
The method involves magnetizing a tracer such as the glucose pyruvate using hyperpolarization (see illustration below).
When the magnetic tracer is injected into the patient, it is absorbed into the body cells. The hyperpolarized tracer increases the MRI signal by a factor of 20,000 or more, allowing cell metabolism to be monitored. Cancer cells in particular reveal themselves in the images.
“Cancer cells have a high metabolism and will therefore convert sugars more quickly than other cells. When the cells break down pyruvate, several different metabolites—degradation products—are formed, including lactate. We can go in and measure the lactate signal, and because it’s magnetic, it will result in areas of the MR image being lit up strongly. The more active the cells are, the more pyruvate they will convert into lactate. The more lactate produced, the more cells they illuminate on the MRI scan. This enables doctors to see how active the cancer cells in a tumour are before and after a given treatment,” says Jan Henrik Ardenkjær-Larsen.
He points out that the method is harmless and gentler than other diagnosis procedures—e.g. biopsy or injection of radioactive trace elements.
Milestone for medical imaging
At the end of 2017, a Danish hospital—Skejby Hospital—was authorized to use hyperpolarized MRI in patients with pancreatic cancer.
Prior to that time, the method had only been tested on animals at both Skejby Hospital and Rigshospitalet in Denmark. Both hospitals work closely together with Jan Henrik Ardenkjær-Larsen’s research group.
“Fortunately our technology has come so far that it is in the hands of doctors who can begin carrying out clinical studies in humans. It is a milestone for the method, as medical imaging is extremely important for diagnosing, characterizing, and following up on diseases,” concludes Professor Ardenkjær-Larsen.
At the HYPERMAG Center of Excellence, researchers are now investigating how Hyperpolarized Metabolic MR can be used to monitor other diseases that are also manifested by metabolic changes in cells—among others. diabetes and cardiovascular diseases.
How hyperpolarized tracers work
Hyperpolarization can magnetize e.g. the harmless sugar pyruvate, so it can be used as a trace element in MRI scans. When injected into a patient before an MRI scan, the MRI signal is boosted by up to a factor of 20,000. The method known as Hyperpolarized Metabolic MRI will be tested for the first time in cancer patients at Skejby Hospital in Denmark in 2018.
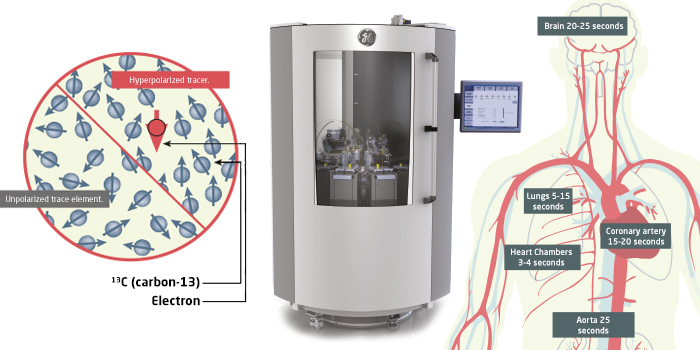
Illustration: Lasse Gorm Jensen
Left image: Before hyperpolarization, the sugar is fortified with carbon-13 if the atomic nucleus is magnetic. A chemical excipient with free electrons (red arrow) is then added.
MIddle image: The actual hyperpolarization process takes place in a machine (polarizer). By cooling the sugar to 1 kelvin (minus 272 degrees Celsius) in a magnetic field, the electrons help to transfer magnetism to the sugar. This process is called dynamic core polarization.
Right image: The trace element is heated lightening fast to room temperature and injected into the patient’s arm. Below we can see the time it takes for the trace element to reach the different organs of the body.
The cells of the body convert the trace element. This results in degradation products (metabolites), which are also magnetic, thus enabling the amounts to be measured by the MRI scan. Since cancer cells have a higher metabolism than normal cells, a high amount of metabolites will detect active cancer cells which appear as brightly lit areas on the MRI image. If the amount of metabolites decreases, it means that the cancer tumour activity is declining.
Data to be collected faster
Time is a critical factor when using magnetized tracer in the MRI scan, as the magnetism only lasts for a few minutes and requires the rapid collection of MR signals.
PhD student Rie Beck Hansen researches in data acceleration—i.e. faster collection of the MRI signals using so-called parallel imaging methods. The methods utilize hardware where MRI signals are absorbed simultaneously (parallel) from multiple coils next to the patient. Many coils provide more angles into the patient, thereby creating an overlap of the recorded data. The overlap can be used to collect fewer MRI signals per coil, which accelerates data collection. Algorithms nonetheless ensure that an accurate MRI image is generated. Rie’s research also includes the development and programming of the MRI scanner software which ensures high-quality MR images. As current methods of collecting MRI signals are too slow, Rie’s research can help create a real basis for hyperpolarized MRI in clinical use.
New generation of polarizers
Magnetizing the contrast medium requires the use of a strong magnetic field, cooling it to minus 272 degrees Celsius with liquid helium, followed by microwave irradation.
Hyperpolarization requires a polarizer, which is expensive to buy and operate. Ideally, to spread the use of imaging using hyperpolarization, there should be a polarizer in every hospital with an MRI scanner. At HYPERMAG, researchers are therefore working to develop a new polarizer which is less costly to buy and operate. The researchers now have a prototype that magnetizes better and faster without using helium. It can reach minus 272 degrees Celsius without using liquid helium simply by employing a cooling unit. It operates at the highest magnetic field yet seen—up to ten Tesla—and can be integrated directly with an MRI scanner.
Contact: Professor Jan Henrik Ardenkjær-Larsen.
More MRI signal to be captured
Electronics capture the MRI signals from the patient during an MRI scan.
The signals are intercepted by small circuits of copper wires, also known as coils. The coils are placed close to the patient during the scan. The more coils, the more signals you can intercept. It can contribute to either better images—or the patient spending less time in the scanner. The challenge, however, is that the coils also contribute noise and error signals that can obscure an MRI image.
So how can we pick up the most of the MR signal with the least possible noise and the fewest possible error signals? PhD student Daniel Højrup Johansen is conducting research into precisely this area. He has developed a preamplifier that disproves the previously held view that it was impossible to remove all fault signals (reciprocal coupling) from the coils.
“We have proven both theoretically and practically that it is possible to construct preamplifiers that minimize noise and remove fault signals from the coils,” says Daniel Højrup Johansen.
The new preamplifiers have been mounted on top of a helmet similar to the one patients wear during head scans. At the same time, Daniel has increased the number of coils on the helmet to 32—instead of the eight or 16 used by researchers. The next step in the project is to test the helmet using phantom scans at Skejby Hospital in North Jutland, Denmark.
“It’s not even certain that 32 coils will produce a better MR image. But it is our job as researchers to challenge the boundaries,” says Daniel Højrup Johansen.
‘On/off button’ for magnetism
If the lifetime of magnetism in the contrast medium can be extended, the distance to the polarizer will no longer be an issue.
The short shelf life of magnetism means that the device (the polarizer), which is responsible for the magnetization of the contrast medium, must be placed close to the MRI scanner. Then the contrast medium can be injected into the patient immediately after being magnetized.
At HYPERMAG, researchers are working on developing a method that can prolong the life of magnetism in the contrast medium. This is done on the basis of new knowledge that the magnetism from electrons can be activated with UV light and deactivated again with heat.
Turning the magnetism of the electrons ‘on and off’ in this way would allow doctors to hyperpolarize the contrast medium long before use—just as it can be transported—doing away with the need for hyperpolarization to take place right next to the MRI scanner.
Contacts: Postdoc Andrea Capozzi and PhD student Christine Pepke Gunnarsson.